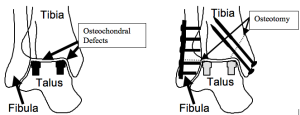
Osteochondral defects and osteonecrosis affect both children and adults. Displacement or collapse of the fragment of bone leads to cartilage damage and eventual ankle arthritis. Transplantation is indicated for extremely large lesions and those with continued pain following other surgical treatments. This can be performed on an outpatient or an inpatient basis, and it’s a procedure Dr. Silverman has performed for many satisfied patients.
Are you experiencing pain or discomfort related to an osteochondral defect or osteonecrosis?
If so, let Dr. Silverman help.
For more information about osteochondral defect surgery, keep reading.
What Happens Before Osteochondral Surgery?
The surgical center will provide specific instructions for how you can prepare for surgery and what to expect when you arrive at the clinic. The day of surgery you will receive regional anesthesia known as a popliteal nerve block. This is a procedure performed by the anesthesiologist prior to surgery. You will be placed on your stomach and a small needle is used to inject Novocain-like medication around the nerve in your leg. It gives complete pain relief that lasts for 12 to 36 hours. People report extraordinary satisfaction with this type of anesthesia. You will be given sedatives during the surgery. Occasionally, general anesthesia is required. You will receive antibiotics just before surgery to help prevent infection.
What Happens During Osteochondral Surgery?
A tourniquet will be placed around your calf and the incisions will be strategically placed. A precise ankle bone osteotomy is performed and the osteochondral defect site is removed with a special coring device. An exactly matched cartilage and bone plug is harvested from your knee (autograft) or from a cadaver talus (allograft) and implanted within defect sites. The osteotomy is fixed with plates and screws. Ligaments and tendons are repaired as necessary. X-rays taken during the surgery confirm the correction, and then the wounds are closed with staples and sutures.
What Happens After Osteochondral Surgery?
You will be permitted to leave the surgical center once your anesthesiologist is satisfied that you have recovered. Some patients need an overnight stay. During this recovery time your family member may take your prescription to the nearest pharmacy. You will be given crutches. Take your narcotic pain control medications during this early post-operative period. Remember post operative pain is much easier to control with prevention. Call to schedule your post-operative visit when you feel able.
Osteoarticular Transplantation General Recovery Timeline
This timeline is a general guideline. Your post-operative course may vary.
| Elevation | 23 hours / day for 10 days; swelling may last over 4 months. |
| Motion | Move your toes and knee when the block resolves. This will decrease pain, swelling and improve healing. Begin ankle motion at 2 weeks. |
| Walking | Begin weight bearing at 6 weeks in the fracture brace if you are given permission. Once the osteotomy heals you may wean out of the brace. |
| Bathing | Keep cast dry. Use a Xerosox. There are no restrictions after the cast is removed. |
| Dressing | After 2 weeks apply Pedifix Compression Anklet or Ace Wrap under the brace. |
| Pain Control | Expect to use strong narcotics for the first 3-5 days. Wean off as soon as you are comfortable using Tylenol or Ultram (Rx only). |
| Work | Return depends on specific demands. It is safe to return to sedentary work at 10 days post-op. Return to heavy labor will take at least 3 months. |
| Driving | Patients with left foot surgery may drive an automatic transmission. Patients with right foot surgery must wait until healing is adequate and they feel safe. |
| Routine Clinic Visits | |
| 2 weeks | XR, Cast and staple removal; Apply Fracture brace |
| 6 weeks | XR, Earliest time of bone healing to permit time out of boot and begin Physical therapy. The time to return for your next visit varies significantly. |
| 3-4 months | XR, Return for recheck; Strength improves over then next year. Minimal feelings of discomfort may linger, your overall comfort level improves over a year. Hardware may be removed if it is bothersome. |
| ********** | If at any time during your post-operative period you notice any drainage or foul odor from your incision, a temperature of more than 100.4 degrees and/or increased swelling or tenderness, you should contact our office. |
If you have troublesome swelling after cast removal you may order a Pedifix Compression Anklet under Ankle Sprain/ Pain. For more helpful tips, check out these rehab exercise videos that will help you recover, or reach out to Dr. Silverman for more information!