A Lisfranc injury involves a combination of fractures and dislocations of the bones and joints in the midfoot. When one of the bones in the midfoot is broken, or one of the ligaments torn, the arch will collapse, guaranteeing arthritis in the midfoot. The collapsed arthritic midfoot is one of the most challenging reconstructions in ankle and foot surgery. Satisfaction rates after surgery are low despite the pain control obtained as it just never “feels right” and the push-off power is difficult to generate. Therefore, midfoot fracture dislocations are almost always treated surgically. 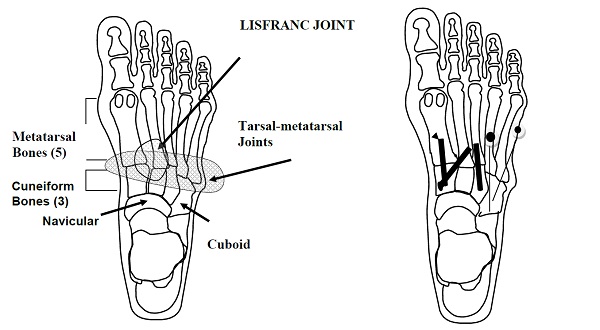
Are you experiencing midfoot pain or have you been diagnosed with a Lisfranc injury?
If so, let Dr. Silverman help. For more information about Lisfranc injuries and treatment, keep reading.
What Happens Before Surgery For Lisfranc Injuries?
Your doctor will give you specific care instructions for how to prepare in the days and weeks leading up to your Lisfranc procedure.
What Happens During Surgery For Lisfranc Injuries?
You will be given antibiotics just before surgery to help prevent infection. During surgery a tourniquet will be placed around your calf. The fracture and dislocations are reduced and stabilized. A primary fusion is performed if the joint is damaged beyond repair. X-Rays are then taken to confirm bone position and wounds are closed with stitches. Finally, a sterile dressing and cast are applied.
What Happens After Surgery For Lisfranc Injuries?
You will be permitted to leave the surgical center once your anesthesiologist is satisfied that you have recovered. During this recovery time your family member may take your prescription to the nearest pharmacy. You will be given crutches and a walking boot. Take your narcotic pain control medication before falling asleep or as you feel the “numbing” effect wear off. Remember, post operative pain is much easier to control with prevention. Call to schedule your post-operative visit for two weeks after surgery when you feel able.
Lisfranc Surgery General Recovery Timeline
This timeline is a general guideline. Your post-operative course may vary.
| Elevation | 23 hours / day for 3 days; then keep elevated as needed. Swelling may last over 4 months. |
| Motion | Move your toes and knee when the block resolves. This will decrease pain, swelling, and improve healing. |
| Walking | If you are healing well I will permit you to begin heel weight bearing at 6 weeks in a fracture brace. |
| Bathing | Keep cast dry. Use a DryPro waterproof cast bag. There are no restrictions after the cast is removed. |
| Pain Control | Expect to use strong narcotics for the first 3-5 days. Wean off as soon as you are comfortable using Tylenol or Ultram (Rx only). NSAIDS will slow healing. |
| Work | Return depends on specific demands. It is safe to return to sedentary work at 10 days post-op. Return to heavy labor and sports will take at least 3 months. |
| Driving | Patients with left foot surgery may drive an automatic transmission. Patients with right foot surgery must wait until healing is adequate and they feel safe. |
Routine Clinic Visits
| 2 weeks | X-ray, cast and staple removal. |
| 6 weeks | X-ray, the earliest time of bone healing to permit weight bearing activity. The time to return for your next visit varies significantly. |
| 14 weeks | X-ray, plan removal of hardware. |
| 4-6 months | Return for recheck. Strength improves over then next year. Minimal feelings of discomfort may linger, your overall comfort level improves over a year. |
| ********** | If at any time during your post-operative period you notice any drainage or foul odor from your incision, a temperature of more than 100.4 degrees and/or increased swelling or tenderness, you should contact our office. |
For more helpful tips, check out these rehab exercise videos that will help you recover, or reach out to Dr. Silverman for more information!