 The following blog is a guest post from Danielle K. Roberts, a medicare insurance expert who writes regularly for a number of online publications, including Forbes. Learn more about Danielle and learn about her insurance insights on her website.
The following blog is a guest post from Danielle K. Roberts, a medicare insurance expert who writes regularly for a number of online publications, including Forbes. Learn more about Danielle and learn about her insurance insights on her website.
Foot problems and pain impact about one in four Americans. With so much wear and tear on the feet every day, it’s no surprise seniors fall victim to foot problems. In some cases, foot problems can require help from a podiatrist to manage and treat symptoms.
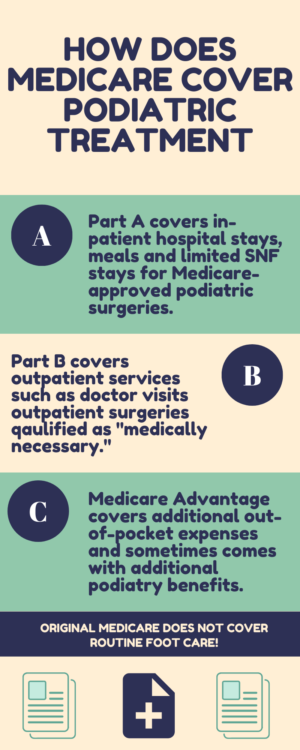
A podiatrist is a doctor who specializes in treating ankles and feet. Adults, as they age, are subject to a higher risk of long-lasting foot conditions, especially if there is another pre-existing disease such as diabetes. When it comes to Medicare, not all procedures, treatment and equipment are covered. In most cases, Medicare won’t cover routine foot care at all.
However, Medicare does cover podiatric treatment under the right circumstances.
Podiatry Services Available Under Medicare
Medicare will not cover routine foot care unless you have another health condition that requires it such as diabetic neuropathy. However, if a particular podiatry service is considered “medically necessary” to treat or diagnose another medical condition, Medicare will cover that service. Circumstances such as bunion deformities, heel spurs and hammertoes tend to be Medicare-approved for coverage of treatment.
Medicare will provide coverage for routine procedures and services from a podiatrist if there is an underlying health condition such as diabetes. Every six months, diabetes patients can get a foot exam as long as they have seen a podiatrist for another reason within those six months.
Additionally, if a patient has peripheral vascular disease, routine podiatry services may be covered by Medicare. Other diseases and conditions such as arteriosclerosis, Buerger’s disease and peripheral neuropathies may also qualify for routine foot coverage under Medicare.
Payment Through Medicare
The average Medicare beneficiary gets podiatry care as an outpatient. Medicare Part B covers medically necessary outpatient doctor services. Medicare Part B pays its portion of 80% of medical costs after you’ve met your annual deductible. As of 2019, the annual deductible for Part B is $185. After Part B has paid its part, you are responsible for covering the remaining 20% of the allowable charges.
Medicare beneficiaries may also have their Part A benefits play a role in certain podiatry treatments. If you are ever admitted to the hospital as an inpatient for a required surgery to treat a foot condition, Part A will cover your hospital stay after you meet your deductible of $1,364.
The above deductible for your Part A benefits will also cover your first 100 days in a skilled nursing facility (SNF). This is only if your doctor recommends rehab or recovery in a skilled nursing facility. Please note that Medicare only covers your SNF stay if your treatment required you to be at the hospital for at least 3 days. If you’d like to learn about Medicare Part C and whether or not medicare covers prosthetic devices, just follow the links.
Additional Medicare Coverage
Since Original Medicare only covers up to 80% of medical expenses, you may want to look into getting supplemental coverage to reduce potential out-of-pocket spending. Medigap and Medicare Advantage plans can reduce your out-of-pocket costs.
Medicare Supplement plans (also known as Medigap) assist in covering your Part A and Part B deductible, coinsurance and copays. On the other hand, Medicare Advantage plans have the potential to reduce your out-of-pocket medical costs by setting a copayment that may be lower than your regular coinsurance for Part B. Medicare Advantage plans also have the ability to offer other benefits that other plans don’t, like routine foot exams.
If you or a loved one ever has concerns about their Medicare coverage for podiatry treatments, please consult your insurance provider or an insurance broker.